Health security including antimicrobial resistance
Antimicrobial Resistance
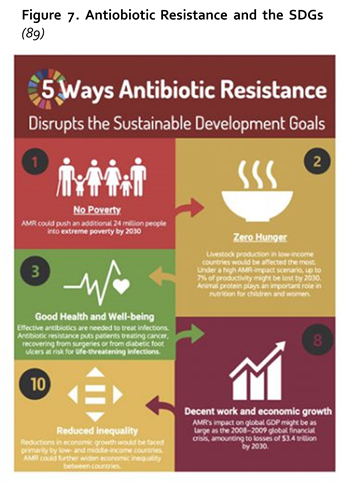
Antimicrobial resistance (AMR), understood as resistance of a bug to one or more chemotherapeutic drugs, is one of the most important contemporary threats to global health, food security and development (86). AMR is associated with longer illness, higher mortality and higher health care costs (87,88), and threatens the success of many disease interventions including surgery, chemotherapy and the fight against malaria, STIs and Tuberculosis (TB). As such, AMR has the potential to disrupt progress towards UHC as well as a number of the SDGs, as outlined in Figure 7 (89).
Figure 7. Antiobiotic Resistance and the SDGs (89)
As an emerging health security challenge, data on AMR is currently relatively limited, in all countries but particularly lower- and middle-income ones. The Global Action Plan on AMR includes a goal to strengthen knowledge through surveillance and research, namely through the Global Antimicrobial Resistance Surveillance System (GLASS) (90). As of December 2018, 71 countries in the world have enrolled in GLASS. Of the 27 countries in the Western Pacific Region, four are enrolled in and reporting AMR data to GLASS (Japan, Malaysia, Philippines and the Republic of Korea) and a further two enrolled in GLASS in 2018 but are yet to start reporting data (Cambodia and Lao PDR) (90).
Current limitations with regards to data quality and representativeness mean that to date GLASS analysis and reports have not attempted to compare AMR status between countries and regions. Data aggregation also remains a major limitation, making analysis of patterns or risk factors linked with age, sex or other factors relevant to gender and equity a challenge. In Japan, Philippines and the Republic of Korea, however sufficient data for analysis is collected on age and gender for at least some of the specimens and pathogens. Furthermore, research from high-income countries, have found moderate to strong associations between national-level income inequality and AMR rates for bacteria (91) and important socioeconomic determinants of antibiotic consumption include population income, demographic structure, density of general practitioners and their remuneration method (92).This is recognized within the Region, where the Regional plan notes that “AMR hits the poor and vulnerable the hardest”, and could push 28 million more people into extreme poverty by 2050, compared to 2017 (93).
Ensuring effective and equitable impact on AMR requires that we understand and acknowledge how men and women, and different groups in society, may be differently at risk of or impacted by AMR and the efforts to address it (94). Despite the limitations of available disaggregated data, Box 5 illustrates ways of looking at AMR to identify how gender and other social determinants impact on efforts to tackle AMR effectively and equitably – bringing the WPR gender and equity lens to all that we do.
References
Feedback
Notification